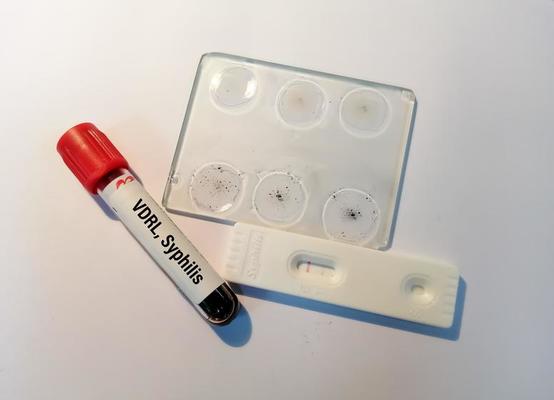
Clinical symptoms of syphilis infection according to the law in Vietnam
Regarding the diagnosis and treatment of syphilis in Vietnam, what are regulations on clinical symptoms of syphilis infection?
Clinical symptoms of syphilis infection according to the law in Vietnam - image from internet
Based on Subsection 2.2.1, Section II of the Guidelines for Diagnosis and Treatment of Syphilis (issued with Decision 5186/QD-BYT in 2021), the clinical symptoms of syphilis infection are as follows:
Clinical symptoms of syphilis infection
a) Primary Syphilis:
- Characteristic clinical manifestation: a single sore (chancre) appearing at the site where the bacteria entered the body, often in the vagina, penis, anus (or in other non-genital locations). The sore usually appears about 3 weeks after infection (around 9-90 days) and may resolve within 3-10 weeks, with or without treatment. Patients may not notice the presence of the sore or may mistake it for a harmless condition.
- If not diagnosed and treated during this stage, the disease progresses to secondary syphilis within 4-8 weeks from the appearance of the initial lesion.
b) Secondary Syphilis:
- Characteristic clinical manifestations: widespread skin and mucosal lesions.
+ Rash: diverse forms of rash may resemble those seen in other conditions. However, syphilitic rash is characterized by its location on the palms, soles of the feet, symmetric distribution, and absence of itching. Lesions can be subtle and easily overlooked on clinical examination.
+ Mucous patches: white patches commonly found on the mucous membranes of the mouth, tongue, and genitals.
+ Condylomata lata: pinkish-red, dome-shaped lesions with a scalloped border (Biett's sign), commonly appearing in warm and moist areas such as the anus and genitals. These are flat, white or grayish lesions that are elevated and result from the spread of syphilitic bacteria from the primary lesion.
- Other non-specific symptoms may include fatigue, fever, lymph node enlargement, hair loss, and headache.
- Secondary syphilis symptoms may resolve spontaneously even without treatment. However, if left untreated, the disease progresses to latent syphilis. Patients in the secondary stage of syphilis are at high risk of transmitting the infection to others.
c) Latent Syphilis:
- No observable signs or clinical symptoms. Therefore, it can only be detected through serological testing.
- Divided into early latent syphilis (infection duration ≤ 2 years) and late latent syphilis (infection duration > 2 years). Patients with uncertain duration of infection should be treated according to the protocol for late latent syphilis. Sexual transmission of syphilis usually occurs during primary syphilis, secondary syphilis, and early latent syphilis. However, transmission from mother to child can occur years after the initial infection.
- If not diagnosed and treated, most patients remain in the latent stage of syphilis. Approximately 25% of patients will progress to tertiary syphilis.
d) Tertiary Syphilis:
- The disease can affect any organ in the body and may occur more than 30 years after the initial infection.
- Characteristic clinical manifestations: neurosyphilis (involvement of the nervous system), cardiovascular syphilis (involvement of the heart and blood vessels), and gummatous syphilis.
+ Neurosyphilis can occur at any stage of the disease, even in the early months. Early neurosyphilis symptoms include acute changes in mental status, meningitis, stroke, cranial nerve dysfunction, auditory and visual abnormalities. Late neurosyphilis may occur 10-30 years or more after infection and is characterized by damage to the posterior roots of the spinal cord, resulting in mild general paralysis.
+ Cardiovascular syphilis typically presents as aortitis (inflammation of the aorta), aortic aneurysm, aortic valve insufficiency, coronary artery stenosis, and in some cases, myocarditis.
+ Gummatous syphilis: a characteristic lesion of tertiary syphilis. Gummata are firm lesions in the subcutaneous tissue, progressing through four stages: initially subcutaneous nodules, which gradually enlarge, become soft, ulcerate, and exude a sticky, rubbery substance resembling gum; the ulcer then extends to involve non-hairy skin, eventually leaving a scar. Gummata can occur in various locations and are commonly found on the face, scalp, buttocks, thighs, and outer aspects of the lower legs. Mucous membranes can also be affected, with common sites being the mouth, lips, hard palate, tongue, and throat. Gummatous lesions in the brain can also occur.
Best regards!